Social work's Elizabeth Anderson receiving Cambia Health Foundation grant for palliative care project
Elizabeth Anderson, a member of the faculty in Western Carolina University’s Department of Social Work, has been chosen by the Cambia Health Foundation to receive a two-year Sojourns Scholar Leadership Program grant totaling $180,000 for a project to identify how to best engage family members of kidney patients in rural areas to ensure that those patients receive palliative care that is consistent with their values.
The foundation recently announced Anderson as one of 12 new grant recipients. It launched the grant program in 2014 with a goal of advancing leadership and innovation in the field of palliative care. Since then, the foundation has awarded more than $9 million to 52 scholars around the nation. Grant recipients in previous years have all been physicians and nurse practitioners, and Anderson is one of the first two social workers to receive the award.

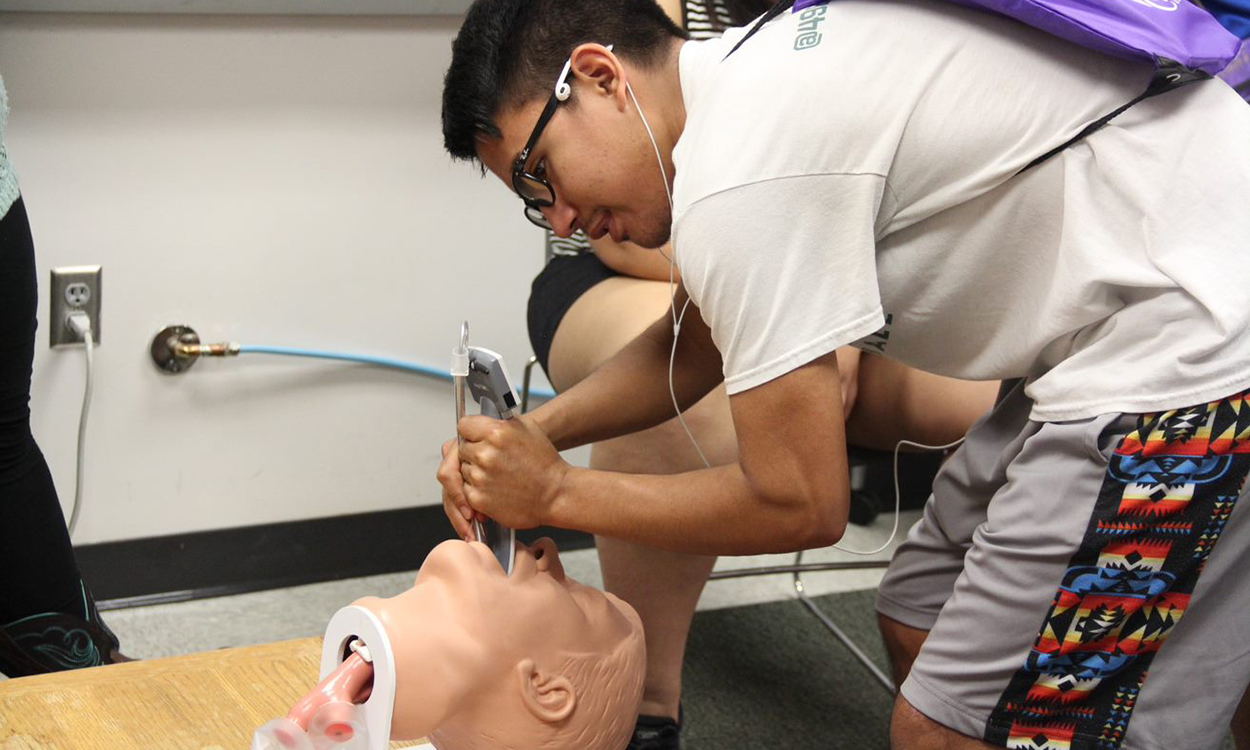
Elizabeth Anderson (left) discusses aspects of her palliative care project with her research assistant Sheena Ledford.
Each of the recipients, who hail from locations ranging from Washington state to Vermont, is expected to engage in an innovative and impactful project in palliative care that also positions the scholar for growth as a national leader in that field. “We are excited to support the development of these emerging leaders and enhance their expertise so that they can influence health care system change,” said Peggy Maguire, president and board chair of the Cambia Health Foundation, the corporate foundation of Cambia Health Solutions. “These palliative care professionals demonstrate that care is better when we focus on what matters to people instead of what’s the matter with them. We hope their leadership will influence compassionate, person-focused care throughout the system.”
Anderson became an assistant professor of social work at WCU in 2016 after previously serving as an adjunct professor. She said she can trace her career journey back to her experiences as a child visiting her grandmother in a nursing home in rural southern Virginia, where she was “haunted by the suffering of elderly patients.” Years later, while working in a nursing home during her first college internship, Anderson said she realized that “much of a person’s suffering was the result of aggressive and often painful attempts to extend life, even when the person could not communicate and had little or no chance for survival.”
“I spent hours in weekly care plan meetings that almost always primarily focused on medication management, rarely invited social work input and almost never included family or caregivers,” she said. But then, after receiving her master’s degree and while working as a hospice social worker and bereavement coordinator, she was “touched by the integrated care team’s approach to the whole person and the inclusion of family members to alleviate suffering through nonmedical venues, recognizing the need to find psychosocial and spiritual relief with the end of life.”
“I began to see not just the patients on my caseload as the client, but the family members that were at their side as well,” she said. “The family members of those I saw in counseling and support groups taught me the importance of family engagement in palliative care.”
 Anderson formerly served as a social worker for Four Seasons Hospice and Palliative
Care in Flat Rock and as social services director for Mid-Atlantic Renal Coalition,
a quality improvement organization for dialysis and transplant facilities in four
states. She earned her doctorate in social work from the University of Tennessee and
now teaches WCU students pursuing bachelor’s and master’s degrees in social work.
For the past two years, she has expanded her work and research in palliative care
for individuals with kidney disease with the Coalition for Supportive Care of Kidney
Patients and George Washington University.
Anderson formerly served as a social worker for Four Seasons Hospice and Palliative
Care in Flat Rock and as social services director for Mid-Atlantic Renal Coalition,
a quality improvement organization for dialysis and transplant facilities in four
states. She earned her doctorate in social work from the University of Tennessee and
now teaches WCU students pursuing bachelor’s and master’s degrees in social work.
For the past two years, she has expanded her work and research in palliative care
for individuals with kidney disease with the Coalition for Supportive Care of Kidney
Patients and George Washington University.
Anderson said her upcoming project will focus on the question: “What is the best approach to family engagement in palliative care for rural patients with kidney disease?” She hopes to find out the perceptions, desires and needs of family members of kidney patients when it comes to palliative care; organize a meeting of local stakeholders that will include the patients, their families and providers to discuss the best approach for engaging the family members in palliative care; and then develop a best-practice tool for providers to use in engaging the families in that care. “A byproduct of this study is to raise the consciousness of the greater community on the burgeoning need for rural palliative care for patients with kidney disease,” she said.
Anderson said a variety of health care disparities that can be found in Western North Carolina, a region that is considered medically underserved, make the area more vulnerable to medical care that is incongruent with the residents’ individual values and beliefs. “With a severe shortage of health care professionals and long travel times in rural Western North Carolina, it is difficult to meet the palliative care needs of any patient or family member, and particularly those with kidney disease,” she said.
Anderson will be joined in her project by research assistant Sheena Ledford, a second-year student in WCU’s master’s degree program in social work and native of WNC.
For more information, contact Anderson at 828-227-3889 or ebanderson@wcu.edu.